1. Choose the correct option
Question (A).
Which one of the following organisms would spend maximum energy in the production of nitrogenous waste?
a. Polar bear
b. Flamingo
c. Frog
d. Shark
Answer:
b. Flamingo
Question (B).
In human beings, uric acid is formed due to metabolism of __________.
a. amino acids
b. fatty acids
c. creatinine
d. nucleic acids
Answer:
d. nucleic acids
Question (C).
Visceral layer : Podocytes :: PCT : _______
a. Cilliated cells
b. Squamous cells
c. Columnar cells
d. Cells with brush border
Answer:
d. Cells with brush border
Question (D).
Deproteinised plasma is found in __________.
a. Bowman’s capsule
b. Descending limb
c. Glomerular capillaries
d. Ascending limb
Answer:
a. Bowman’s capsule, b. Descending limb, d. Ascending limb
Question (E).
Specific gravity of urine would _______ if level of ADH increases.
a. remain unaffected
b. increases
c. decreases
d. stabilise
Answer:
b. increases
Question (F).
What is micturition?
a. Urination
b. Urine formation
c. Uremia
d. Urolithiasis
Answer:
a. Urination
Question (G).
Which one of the following organisms excrete waste through nephridia?
a. Cockroach
b. Earthworm
c. Crab
d. Liver Fluke
Answer:
c. Crab
Question (H).
Person suffering from kidney stone is advised not to have tomatoes as it has _______.
a. seeds
b. lycopene
c. oxalic acid
d. sour taste
Answer:
c. oxalic acid
Question (I).
Tubular secretion does not take place in ________.
a. DCT
b. PCT
c. collecting duct
d. Henle’s loop
Answer:
b. PCT
Question (J).
The minor calyx ____________.
a. collects urine
b. connects pelvis to ureter
c. is present in the cortex
d. receives column of Bertini
Answer:
a. collects urine
Question (K).
Which one of the followings is not a part of human kidney?
a. Malpighian body
b. Malpighian tubule
c. Glomerulus
d. Loop of Henle
Answer:
b. Malpighian tubule
Question (L).
The yellow colour of the urine is due to presence of ___________
a. uric acid
b. cholesterol
c. urochrome
d. urea
Answer:
c. urochrome
Question (M).
Hypotonic filtrate is formed in _______
a. PCT
b. DCT
c. LoH
d. CT
Answer:
a. PCT
Question (N).
In reptiles, uric acid is stored in _____
a. cloaca
b. fat bodies
c. liver
d. anus
Answer:
a. cloaca
Question (O).
The part of nephron which absorbs glucose and amino acid is______
a. collecting tubule
b. proximal tubule
c. Henle’s loop
d. DCT
Answer:
b. proximal tubule
Question (P).
Bowman’s capsule is located in kidney in the ________
a. cortex
b. medulla
c. pelvis
d. pyramids
Answer:
a. cortex
Question (Q).
The snakes living in desert are mainly__________
a. aminotelic
b. ureotelic
c. ammonotelic
d. uricotelic
Answer:
d. uricotelic
Question (R).
Urea is a product of breakdown of ___________
a. fatty acids
b. amino acids
c. glucose
d. fats
Answer:
b. amino acids
Question (S).
Volume of the urine is regulated by__________
a. aldosterone
b. ADH
c. both a and b
d. none
Answer:
Question 2.
Answer the following questions
Question (A).
Doctors say Mr. Shaikh is suffering from urolithiasis. How it could be explained in simple words?
Answer:
Urolithiasis is the condition of having calculi in the urinary tract (which also includes the kidneys), which may pass into urinary bladder.
Question (B).
Anitaji needs to micturate several times and feels very thirsty. This is an indication of change in permeability of certain part of nephron. Which is this part?
Answer:
- Need to micturate several times (polyuria) and feeling very thirsty (polydipsia) is a symptom of diabetes insipidus (imbalance of fluids in the body).
- ADH prevents diuresis and due to absence of ADH, large amount of dilute urine is excreted.
- ADH stimulates reabsorption of water from last part of DCT and entire collecting duct by increasing the permeability of cells.
- If the permeability of these cells changes, it will result in increase in urine volume (frequent micturition) and increase in the osmolarity of blood. An imbalance in volume and osmolarity of body fluids increases thirst.
[Note: Water is reabsorbed by osmosis in PCT, DCT and descending limb of loop of Henle)
Question (C).
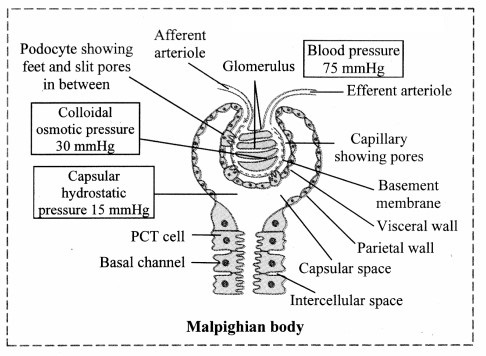
Effective filtration pressure was calculated to be 20 mm Hg; where glomerular hydrostatic pressure was 70 mm of Hg. Which other pressure is affecting the filtration process? How much is it?
Answer:
The other pressure affecting the filtration process is osmotic pressure of blood and filtrate hydrostatic pressure. Commonly effective filtration pressure (EFP) is represented as;
EFP = Glomerular Hydrostatic pressure in glomerulus – (Osmotic pressure of blood + Filtrate Hydrostatic pressure)
If EFP = 20 mmHg and Glomerular Hydrostatic pressure = 70 mmHg
20 = 70 – (Osmotic pressure of blood + Filtrate hydrostatic pressure)
∴ (Osmotic pressure of blood + Filtrate hydrostatic pressure) = 70-20
Then (Osmotic pressure of blood + Filtrate Hydrostatic pressure) = 50 mmHg .
[Note: Given values are insufficient to calculate the exact osmotic pressure of blood and filtrate hydrostatic pressure. The sum of the two values can be calculated to be 50 mmHg ]
Question (D).
Name any one guanotelic organism.
Answer:
Spiders, scorpions and penguins are guanotelic organisms as they excrete guanine.
Question (E).
Why are kidneys called ‘retroperitoneal’?
Answer:
Kidneys are located in abdomen. Kidneys are not surrounded by peritoneum instead they are located posterior to it. Thus, kidneys are called retroperitoneal.
Question (F).
State role of liver in urea production.
Answer:
- Ammonia formed during the breakdown of amino acids is converted into urea in the liver of ureotelic animals.
- This conversion takes place by the help of the ornithine / urea cycle.
- 3 ATP molecules are used to produce one molecule of urea using the ornithine/ urea cycle. Since, the liver contains carrier molecules and enzymes necessary for urea cycle, it plays a major role in urea production.
Question (G).
Why do we get bad breath after eating garlic or raw onion?
Answer:
- Raw onion and garlic contain volatile sulphur-containing compounds.
- Sulphur-containing compounds have a distinctive odour which remain in the mouth after consumption of onion and garlic.
- Also, volatile compounds (like certain sulphur containing compounds) in foodstuffs are generally excreted through the lungs and may result in bad breath.
3. Answer the following questions
Question (A).
John has two options as treatment for his renal problem : Dialysis or kidney transplants. Which option should he choose? Why?
Answer:
- If John has two options of dialysis and kidney transplant, readily available he must opt for kidney transplant.
- A kidney transplant, if successful, can improve the quality of life of a patient and reduce the risk of death.
- The patient would not have to endure frequent dialysis procedures. Repeated visits for dialysis takes time and may not allow the patient to perform normal activities or go to office regularly.
- Dialysis is regarded as a holding measure until kidney transplant can be performed or a supportive measure in those for whom a transplant would be inappropriate. However, dialysis cannot replace all the functions of a normal kidney such as production of hormones like erythropoietin, calcitriol and renin. Hence, if John has an option of kidney transplant, he must opt for it.
Question (B).
Amphibian tadpole can afford to be ammonotelic. Justify.
Answer:
- Tadpole (larval stage of life cycle of amphibian) is aquatic. They are ammonotelic as they excrete nitrogenous waste in the form of ammonia.
- Ammonia is very toxic and requires large amount of water for its elimination.
- It is readily soluble in water and diffuses across the body surface and into the surrounding water.
- Also, the water lost during excretion can be made up through the surrounding water in ammonotelic organisms.
Hence, amphibian tadpole can afford to be ammonotelic.
Question (C).
Birds are uricotelic in nature. Give reason.
Answer:
- Birds are capable of converting ammonia into uric acid by ‘inosinic acid pathway’ in their liver.
- Uric acid is least toxic and hence, it can be retained in the body for some time.
- It is least soluble water hence, negligible amount of water is required for its elimination.
- This mode of excretion can also help reduce body weight (an adaptation for flight) and those animals which
need to conserve more water follow uricotelism.
Hence, in order to conserve water as an adaptation for flight, birds are uricotelic in nature.
Question 4.
Write the explanation in your word
Question (A).
Nitya has been admitted to hospital after heavy blood loss. Till proper treatment could be given; how did Nitya’s body must have tackled the situation?
Answer:
- Heavy blood loss is called haemorrhage. In case of haemorrhage or severe dehydration, the osmoreceptors stimulate Antidiuretic hormone (ADH) secretion.
- ADH is important in regulating water balance through the kidneys. For detailed mechanism of reabsorption by ADH:
Regulating water reabsorption through ADH:
Hypothalamus in the midbrain has special receptors called osmoreceptors which can detect change in osmolarity (measure of total number of dissolved particles per liter of solution) of blood.
If osmolarity of blood increases due to water loss from the body (after eating namkeen or due to sweating), osmoreceptors trigger release of Antidiuretic hormone (ADH) from neurohypophysis (posterior pituitary). ADH stimulates reabsorption of water from last part of DCT and entire collecting duct by increasing the permeability of cells.
This leads to reduction in urine volume and decrease in osmolarity of blood.
Once the osmolarity of blood comes to normal, activity of osmoreceptor cells decreases leading to decrease in ADH secretion. This is called negative feedback.
In case of hemorrhage or severe dehydration too, osmoreceptors stimulate ADH secretion. ADH is important in regulating water balance through kidneys.
In absence of ADH, diuresis (dilution of urine) takes place and person tends to excrete large amount of dilute urine. This condition called as diabetes insipidus.
[Note: Hypothalamus is a part of forebrain]
Another regulatory mechanism that must have been activated is RAAS. For detailed mechanism of electrolyte reabsorption:
Electrolyte reabsorption through RAAS:
Another regulatory mechanism is RAAS (Renin Angiotensin Aldosterone System) by Juxta Glomerular Apparatus (JGA).
Whenever blood supply (due to change in blood pressure or blood volume) to afferent arteriole decreases (e.g. low BP/dehydration), JGA cells release Renin. Renin converts angiotensinogen secreted by hepatocytes in liver to Angiotensin I. ‘Angiotensin-converting enzyme’ further modifies Angiotensin I to Angiotensin II, the active form of hormone. It stimulates adrenal cortex to release another hormone called aldosterone that stimulates DCT and collecting ducts to reabsorb more Na+ and water, thereby increasing blood volume and pressure.
Question 5.
Complete the diagram / chart with correct labels / information. Write the conceptual details regarding it
Question (A).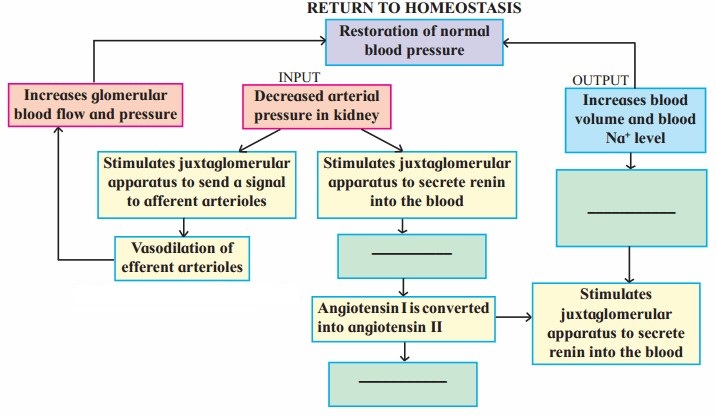
Answer: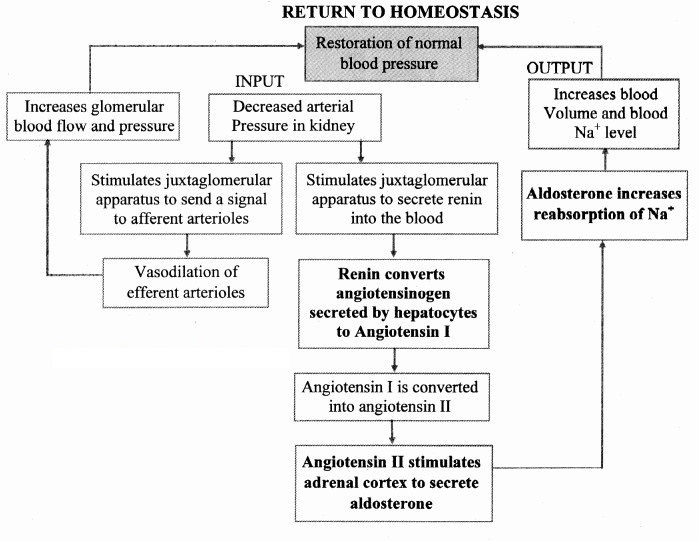
The composition of urine depends upon food and fluid consumed by an individual. There are two ways in which it the composition is regulated. They are as follows:
i. Regulating water reabsorption through ADH
ii. Electrolyte reabsorption though RAAS
iii. Atrial Natriuretic Peptide
i. Regulating water reabsorption through ADH:
Hypothalamus in the midbrain has special receptors called osmoreceptors which can detect change in osmolarity (measure of total number of dissolved particles per liter of solution) of blood.
If osmolarity of blood increases due to water loss from the body (after eating namkeen or due to sweating), osmoreceptors trigger release of Antidiuretic hormone (ADH) from neurohypophysis (posterior pituitary). ADH stimulates reabsorption of water from last part of DCT and entire collecting duct by increasing the permeability of cells.
This leads to reduction in urine volume and decrease in osmolarity of blood.
Once the osmolarity of blood comes to normal, activity of osmoreceptor cells decreases leading to decrease in ADH secretion. This is called negative feedback.
In case of hemorrhage or severe dehydration too, osmoreceptors stimulate ADH secretion. ADH is important in regulating water balance through kidneys.
In absence of ADH, diuresis (dilution of urine) takes place and person tends to excrete large amount of dilute urine. This condition called as diabetes insipidus.
[Note: Hypothalamus is a part of forebrain]
ii. Electrolyte reabsorption through RAAS:
Another regulatory mechanism is RAAS (Renin Angiotensin Aldosterone System) by Juxta Glomerular Apparatus (JGA).
Whenever blood supply (due to change in blood pressure or blood volume) to afferent arteriole decreases (e.g. low BP/dehydration), JGA cells release Renin. Renin converts angiotensinogen secreted by hepatocytes in liver to Angiotensin I. ‘Angiotensin converting enzyme’ further modifies Angiotensin I to Angiotensin II, the active form of hormone. It stimulates adrenal cortex to release another hormone called aldosterone that stimulates DCT and collecting ducts to reabsorb more Na+ and water, thereby increasing blood volume and pressure.
iii. Atrial natriuretic peptide (ANP): A large increase in blood volume and pressure stimulates atrial wall to produce atrial natriuretic peptide (ANP). ANP inhibits Na+ and Cl– reabsorption from collecting ducts inhibits release of renin, reduces aldosterone and ADH release too. This leads to a condition called Natriuresis (increased excretion of Na+ in urine) and diuresis.
Question (B).
Answer: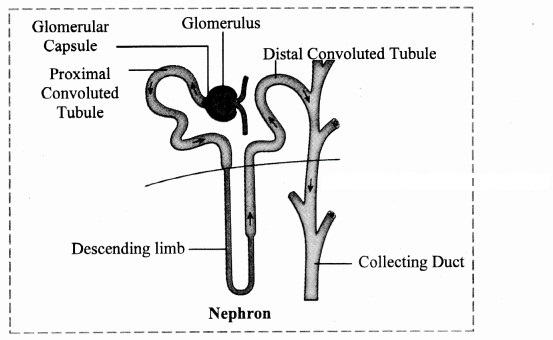
- Nephrons are structural and functional units of kidney.
- Each nephron consists of a 4 – 6 cm long, thin-walled tube called the renal tubule and a bunch of capillaries known as the glomerulus.
- The wall of the renal tubule is made up of a single layer of epithelial cells.
- Its proximal end is wide, blind, cup-like and is called as Bowman’s capsule, whereas the distal end is open.
- The nephron is divisible into Ilowman’s capsule, neck, proximal convoluted tubule (PCT), Loop of Henle (LoH), distal convoluted tubule (DCT) and collecting tubule (CT).
- The glomerulus is present in the cup-like cavity of Bowman’s capsule and both are collectively known as renal corpuscle or Malpighian body.
Question (C)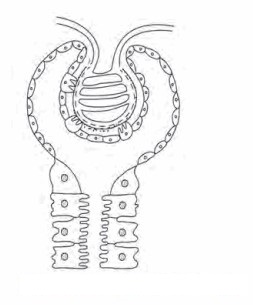
Answer:
Nephron is the structural and functional unit of kidney.
Structure of nephron:
A nephron (uriniferous tubule) is a thin walled, coiled duct, lined by a single layer of epithelial cells. Each nephron is divided into two main parts:
i. Malpighian body
ii. Renal tubule
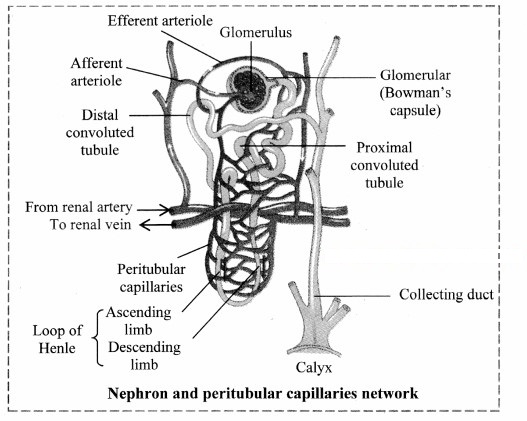
i. Malpighian body: Each Malpighian body is about 200pm in diameter and consists of a Bowman’s capsule and glomerulus.
a. Glomerulus:
Glomerulus is a bunch of fine blood capillaries located in the cavity of Bowman’s capsule.
A small terminal branch of the renal artery, called as afferent arteriole enters the cup cavity (Bowman capsule) and undergoes extensive fine branching to form network of several capillaries. This bunch is called as glomerulus.
The capillary wall is fenestrated (perforated).
All capillaries reunite and form an efferent arteriole that leaves the cup cavity.
The diameter of the afferent arteriole is greater than the efferent arteriole. This creates a high hydrostatic pressure essential for ultrafiltration, in the glomerulus.
b. Bowman’s capsule:
It is a cup-like structure having double walls composed of squamous epithelium.
The outer wall is called as parietal wall and the inner wall is called as visceral wall.
The parietal wall is thin consisting of simple squamous epithelium.
There is a space called as capsular space / urinary space in between two walls.
Visceral wall consists of special type of squamous cells called podocytes having a foot-like pedicel. These podocytes are in close contact with the walls of capillaries of glomerulus.
There are small slits called as filtration slits in between adjacent podocytes.
ii. Renal tubule:
a. Neck:
The Bowman’s capsule continues into the neck. The wall of neck is made up of ciliated epithelium. The lumen of the neck is called the urinary pole. The neck leads to proximal convoluted tubule.
b. Proximal Convoluted Tubule :
This is highly coiled part of nephron which is lined by cuboidal cells with brush border (microvilli) and surrounded by peritubular capillaries. Selective reabsorption occurs in PCT. Due to convolutions (coiling), filtrate flows slowly and remains in the PCT for longer duration, ensuring that maximum amount of useful molecules are reabsorbed.
c. Loop of Henle :
This is ‘U’ shaped tube consisting of descending and ascending limb.
The descending limb is thin walled and permeable to water and lined with simple squamous epithelium.
The ascending limb is thick walled and impermeable to water and is lined with simple cuboidal epithelium.
The LoH is surrounded by capillaries called vasa recta.
Its function is to operate counter current system – a mechanism for osmoregulation.
The ascending limb of Henle’s loop leads to DCT.
d. Distal convoluted tubule:
This is another coiled part of the nephron.
Its wall consists of simple cuboidal epithelium.
DCT performs tubular secretion / augmentation / active secretion in which, wastes are taken up from surrounding capillaries and secreted into passing urine.
DCT helps in water reabsorption and regulation of pH of body fluids.
e. Collecting tubule:
This is a short, straight part of the DCT which reabsorbs water and secretes protons.
The collecting tubule opens into the collecting duct.
Question (D).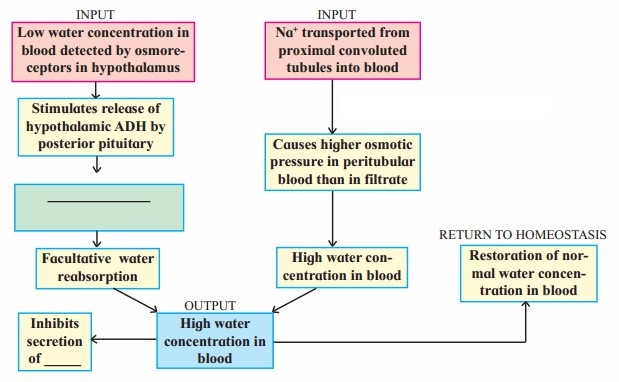
Answer: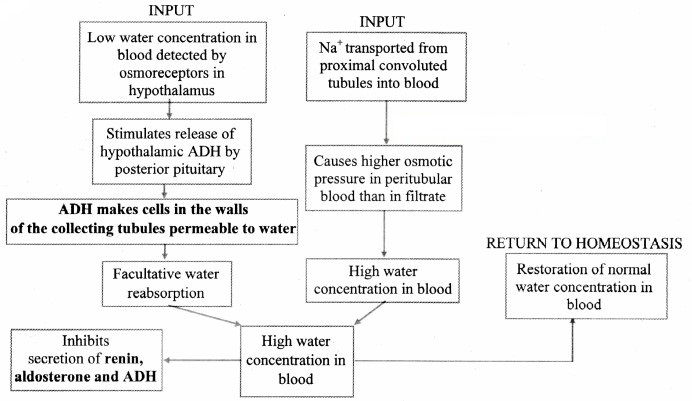
The composition of urine depends upon food and fluid consumed by an individual. There are two ways in which it the composition is regulated. They are as follows:
i. Regulating water reabsorption through ADH
ii. Electrolyte reabsorption though RAAS
iii. Atrial Natriuretic Peptide
i. Regulating water reabsorption through ADH:
Hypothalamus in the midbrain has special receptors called osmoreceptors which can detect change in osmolarity (measure of total number of dissolved particles per liter of solution) of blood.
If osmolarity of blood increases due to water loss from the body (after eating namkeen or due to sweating), osmoreceptors trigger release of Antidiuretic hormone (ADH) from neurohypophysis (posterior pituitary). ADH stimulates reabsorption of water from last part of DCT and entire collecting duct by increasing the permeability of cells.
This leads to reduction in urine volume and decrease in osmolarity of blood.
Once the osmolarity of blood comes to normal, activity of osmoreceptor cells decreases leading to decrease in ADH secretion. This is called negative feedback.
In case of hemorrhage or severe dehydration too, osmoreceptors stimulate ADH secretion. ADH is important in regulating water balance through kidneys.
In absence of ADH, diuresis (dilution of urine) takes place and person tends to excrete large amount of dilute urine. This condition called as diabetes insipidus.
[Note: Hypothalamus is a part of forebrain]
ii. Electrolyte reabsorption through RAAS:
Another regulatory mechanism is RAAS (Renin Angiotensin Aldosterone System) by Juxta Glomerular Apparatus (JGA).
Whenever blood supply (due to change in blood pressure or blood volume) to afferent arteriole decreases (e.g. low BP/dehydration), JGA cells release Renin. Renin converts angiotensinogen secreted by hepatocytes in liver to Angiotensin I. ‘Angiotensin-converting enzyme’ further modifies Angiotensin I to Angiotensin II, the active form of hormone. It stimulates adrenal cortex to release another hormone called aldosterone that stimulates DCT and collecting ducts to reabsorb more Na+ and water, thereby increasing blood volume and pressure.
iii. Atrial natriuretic peptide (ANP): A large increase in blood volume and pressure stimulates atrial wall to produce atrial natriuretic peptide (ANP). ANP inhibits Na+ and Cl– reabsorption from collecting ducts inhibits release of renin, reduces aldosterone and ADH release too. This leads to a condition called Natriuresis (increased excretion of Na+ in urine) and diuresis.
Question (E).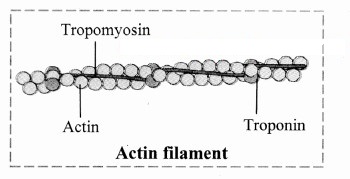
Answer: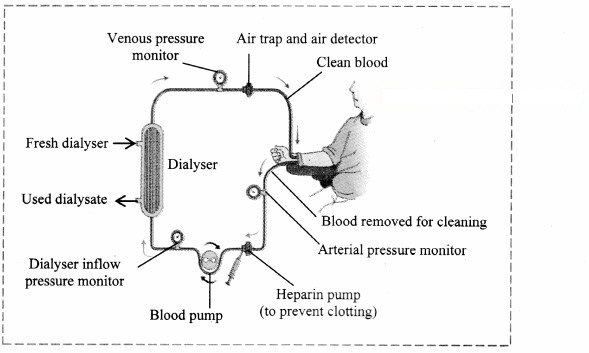
- When renal function of a person falls below 5 – 7 %, accumulation of harmful substances in blood begins. In such a condition the person has to go for artificial means of filtration of blood i.e. haemodialysis.
- In haemodialysis, a dialysis machine is used to filter blood. The blood is filtered outside the body using a dialysis unit.
- In this procedure, the patients’ blood is removed; generally from the radial artery and passed through a cellophane tube that acts as a semipermeable membrane.
- The tube is immersed in a fluid called dialysate which is isosmotic to normal blood plasma. Hence, only excess salts if present in plasma pass through the cellophane tube into the dialysate.
- Waste substances being absent in the dialysate, move from blood into the dialyzing fluid.
- Filtered blood is returned to vein.
- In this process it is essential that anticoagulant like heparin is added to the blood while it passing through the tube and before resending it into the circulation, adequate amount of anti-heparin is mixed.
- Also, the blood has to move slowly through the tube and hence the process is slow.
Question 6.
Prove that mammalian urine contains urea.
Answer:
- Urea is a nitrogenous waste formed by breakdown of protein (deamination of amino acids).
- During this process, amino groups are removed from the amino acids present in the proteins and converted to highly toxic ammonia. The ammonia is finally converted to area through ornithine cycle. Thus, the urea formed is passed to kidneys and excreted out of the body through urine.
- Reabsorption of urea (proximal tubule, collecting ducts) and active secretion of urea (Henle loop) leads to a urea circulation (urea recycling) between the lumen of the nephron and renal medulla, which is an important element of the renal urine concentration.
- About 54 g of urea is filtered per day in the glomerular capsule, of which approximately 30 g is excreted in the urine and 24 g is reabsorbed into blood (assuming GFR is 180 litres/day).
- Urinalysis can help detect the amount of urea in urine (Urine urea nitrogen test, urease test, etc.).
Practical / Project :
Visit to a nearby hospital or pathological laboratory and collect detailed information about different blood and urine tests.
Answer:
Testing the urine is known as urinalysis. It generally has three parts:
- Visual examination: Check sample colour and clearness.
- Dipstick examination: Checks for abnormal amounts of glucose, protein, etc.
- Microscopic examination: Check for presence of RBCs. WBCs, bacteria, crystals, etc.
- Apart from routine urine examination, specific tests may also be done. They are as follows:
- BUN (Blood Urea Nitrogen) Test: It measures the amount of nitrogen in blood and evaluates kidney function.
- Urease Test/ Urea Nitrogen Test: It is done to check the amount of urea in urine sample.
- Urine albumin to creatine ratio (UACR) test: Estimates the amount of albumin in urine.
[Students are expected to collect more information and perform the given activity on their own]
Intext Questions and Answers
Can you recall? (Textbook Page No. 174)
Question 1.
Why are various waste products produced in the body of an organism?
Answer:
Metabolism produces a variety of by-products, some of which need to be eliminated. Such by-produçts are called metabolic waste products.
Question 2.
How are these waste eliminated?
Answer:
Depending on the type of waste product, they are eliminated through various organs of the body:
The various excretory products produced by the human body are as follows:
- Fluids such as water; gaseous wastes like CO2 nitrogenous wastes like ammonia, urea and uric acid, creatinine; minerals; salts of sodium, potassium. calcium, etc. if present in body in excess are excreted through urine, faeces and sweat.
- Pigments formed due to breakdown of haemoglobin like bilirubin (excreted through faeces) and urochrome (eliminated through urine).
- The pigments present in consumed foodstuffs like beet root or excess of vitamins, hormones and drugs.
- Volatile substances present in spices (eliminated through lungs).
Have you ever observed? (Textbook Page No. 174)
Question 1.
When does urine appear deeply coloured?
Answer:
Urine can appear deeply coloured due to various reasons:
- Severe dehydration resulting in production of concentrated urine.
- Consumption of foodstuff like beet root, which contain coloured pigments.
- Some medications can also cause the urine to appear deeply coloured.
Think about it. (Textbook Page No. 174)
Question 1.
Do organisms differ in type of metabolic wastes they produce?
Answer:
Yes, organisms differ in the type of metabolic wastes they produce. Some organisms excrete ammonia while some excrete urea or uric acid as metabolic wastes.
Question 2.
Do environment or evolution have any effect on type of waste produced by an organism?
Answer:
- The theory of evolution proposes that life started in an aquatic environment.
- Aquatic organisms are generally ammonotelic. It is believed that the urea cycle evolved to adapt to a changing environment when terrestrial life forms evolved.
- Arid conditions probably led to the evolution of the uric acid pathway as a means of conserving water.
- However, the correlation between evolution and type of waste production is uncertain.
Question 3.
How do thermoregulation and food habits affect saste production?
Answer:
- To generate heat. endotherms convert the food that they eat into energy through a process called metabolism. Hence, they consume more tì.od in order to meet their energy requirements.
- Also, carnivorous diet contains more proteins than herbivores.
- Consumption of high protein or more food containing proteins can result in production of large amount of nitrogenous waste
- These animals would also require more energy to eliminate the high levels oF nitrogenous wastes which build up when animal protein is digested.
Use your brain power. (Textbookpage No. 175)
Question 1.
Why ammonia is highly toxic?
Answer:
- Ammonia is basic in nature and its retention in the body would disturb the pH of the body.
- An increase in pH would disturb all enzyme catalysed reactions in the body and also make the plasma membrane unstable.
Hence, ammonia is highly toxic to the body.
Find out. (Textbook page No. 175)
You will study about a type of arthritis called gouty arthritis caused due to accumulation of uric acid in joints. Where does uric acid come from in case of ureotelic human beings?
Answer:
- Uric acid produced as a waste product during the normal breakdown of nucleic acids (purines) and certain naturally occurring substances found in foods such as mushrooms. Mackerel, dried beans. etc.
- This uric acid is generally excreted out along with urine.
- If uric acid is produced in excess or not excreted, it accumulates in joints causing gouty arthritis.
Think about it. (Textbook Page No.175)
Endotherms consume more food in order to meet energy requirements. Also, carnivorous diet contains more proteins than herbivorous. Does it affect excretion of nitrogenous waste?
Answer:
- To generate heat, endotherms convert the food that they eat into energy through a process called metabolism. Hence, they consume more food in order to meet their energy requirements.
- Also, carnivorous diet contains more proteins than herbivores.
- Consumption of high protein or more food containing proteins can result in production of large amount of nitrogenous waste.
- These animals would also require more energy to eliminate the high levels of nitrogenous wastes which build up when animal protein is digested.
Observe and Discuss (Textbook Page No. 176)
Question 1.
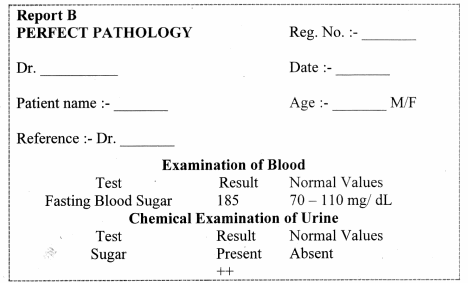
These are blood reports of patients undergoing investigations for kidney function. What is creatinine? What is your observation and opinion about the findings? Why is it used as an index of kidney function?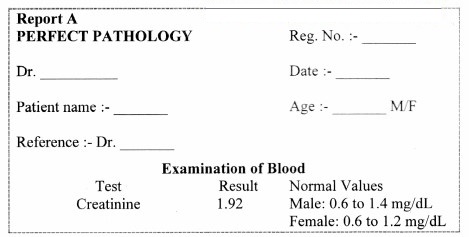
Answer:
i. Creatinine:
- Plasma creatinine is produced from catabolism of creatinine phosphate during skeletal muscle contraction.
- It provides a ready source of high energy phosphate.
ii. Observations and Opinion:
Report A indicates a value of creatinine which is higher than the normal range. This would indicate impaired kidney function.
Report B indicates high fasting blood sugar and detection of sugar in the blood is known as glucosuria. High fasting blood sugar (>126 mg/dL) is usually indicative of diabetes.
iii. Creatinine used as an index of kidney function:
- Normally blood creatinine levels remain steady because the rate of production matches his excretion in urine.
- Hence, plasma creatinine is used as an index of kidney function and its level above normal is an indication of poor renal function.
Think about it. (Textbook Page No. 176)
Question 1.
During summer, we tend to produce less urine, is it so?
Answer:
- Generally, excess water containing wastes is lost from the body in the time of urine. sweat and faeces.
- During summer when the surrounding temperature is high. we also lose a considerable amount of water in the form of sweat.
Thus, the kidneys retain water for maintaining the concentration of body fluids and reduce the amount of water lost through urine.
Question 2.
Marine birds like Albatross spend their life on the sea. That means the water the, drink is salty. how do they manage osnioregulation then?
Answer:
- Marine birds like Albatross have special glands called salt glands near their nostrils.
- These glands are capable of secreting salts by active transport and help to manage osmotic balance,
[Note: The salt glands in Albatross are located in or on the skull in the area of eyes.]
Question 3.
like ectothermic and endothermic animals, do organisms differ in the way they maintain salt balance?
Answer:
Yes, organisms differ in the way they maintain salt balance.
- Animals can be either isosmotic to the surrounding (osmoconformers or control the internal environment independent of external environment (osmoregulators).
- Marine organisms are mostly osmoconfòrmers because their body fluids and external environment are isosmotic in nature while fresh water forms and terrestrial organisms are osmoregulators,
- Generally, most organisms can tolerate only a narrow range of salt concentrations. Such organism are known as stenohaline organisms.
- Organisms which are capable of handling a wide change in salinity are called euryhaline organisms.e.g. Barnacles, clams etc.
Find out. (Textbook Page No 176)
Question 1.
How do freshwater fishes and marine fishes carry out osmoregulation?
Answer:
Osmoregulation is the process of maintaining an internal concentration of salt and water in the body of fishes.
i. Freshwater fishes:
The salt concentration inside the body of freshwater fishes is higher than their surrounding water. Due to this, water enters the body due to osmosis.
If the flow of water into the body is not regulated. fishes would swell and get bigger.
To compensate this, the kidneys produce a large amount of urine,
Excretion of large amounts of urine regulates the level of water in the body hut results in the loss of salts.
Thus, in order to maintain a sufficient salt level, special cells in the gills (chloride cells) take tip ions from
the water, which are then directly transported into the blood.
ii. Marine fishes:
Since the salt content in blood of marine fishes is much lower than that of seawater, they constantly tend to lose water and build up salt.
To replace the water loss, they continually need to drink seawater.
Since their small kidney can only excrete a relatively small amount of urine, salt is additionally excreted through gills, where chloride cells work in reverse as in freshwater fishes.
Make a table. (Textbook Page No. 178)
Question 1.
The details of modes of excretion of nitrogenous wastes.
Answer:
The three main modes of excretion in animals are as follows:
i. Ammonotelism
ii. Ureotelism
iii. Uricotelism
i. Ammonotelism:
- Elimination of nitrogenous wastes in the form of ammonia is called as ammonotelism.
- Ammonia is basic in nature and hence it can disturb the pH of the body, if not eliminated immediately.
- Any change in pH would disturb all enzyme catalyzed reactions in the body and would also make the plasma membrane unstable.
- Ammonia is readily soluble in water and needs large quantity of water to dilute and reduce its toxicity.
- This is however an energy saving mechanism of excretion and hence all animals that have plenty of water available for dilution of ammonia, excrete nitrogenous wastes in the form of ammonia.
- Animals that follow this mode of excretion are known as ammonotelic animals.
- 1 gm ammonia needs about 300 – 500 ml of water for elimination.
- Ammonotelic animals excrete ammonia through general body surface (skin), gills and kidneys.
e.g. Ammonotelism is found in aquatic invertebrates, bony fishes, and aquatic / larval amphibians. Animals without excretory system (Protozoa) are also ammonotelic.
ii. Ureotelism:
- Elimination of nitrogenous wastes in the form of urea is called as ureotelism.
- Urea is comparatively less toxic and less water-soluble than ammonia. Hence, it can be concentrated to some extent in body.
- The body requires less water for elimination.
- Since it is less toxic and less water soluble, ureotelism is suitable for animals that need to conserve water to some extent. Hence, ureotelism is common in terrestrial animals, as they have to conserve water.
- It takes about 50 ml H2O for removal of 1 gm NH2 in form of urea.
- Ureotelic animals generally convert ammonia to urea in the liver by operating ornithine / urea cycle in which 3 ATP molecules are used to produce one molecule of urea.
e.g. Mammals, cartilaginous fishes (sharks and rays), many aquatic reptiles, most of the adult amphibians, etc. are ureotelic.
iii. Uricotelism:
- Elimination of nitrogenous wastes in the form of uric acid is called as uricotelism.
- Uric acid is least toxic and hence, it can be retained in the body for some time in concentrated form.
- It is least soluble in water. Hence there is minimum (about 5 – 10 ml for 1 gm) or no need of water for its elimination.
- Those animals which need to conserve more water follow uricotelism. However, these animals need to spend more energy.
- Ammonia is converted into uric acid by ‘inosinic acid pathway’ in the liver of birds, e.g. Birds, some insects, many reptiles, land snails, are uricotelic.
| No. | Ureotelism | Uricotelism |
| i. | It is the elimination of nitrogenous waste in the form of urea. | It is the elimination of nitrogenous waste in the form of uric acid. |
| ii. | Excretion of urea requires less (moderate ) amount of water. | Excretion of uric acid requires negligible amount of water. |
| iii. | Removal of 1 gm of urea requires 50 ml of water. | Removal of 1 gm of uric acid requires 5 – 10 ml of |
| iv. | rea is less toxic. | Uric acid is least toxic. |
| e.g. | It is generally seen in terrestrial animals. Mammals, cartilaginous fishes (sharks and rays), many aquatic reptiles, most adult amphibians, etc. | It is seen in birds, some insects, many reptiles, land snails, etc. |
| No. | Ammonotelism | Uricotelism |
| i. | It is the elimination of nitrogenous waste in the form of ammonia. | It is the elimination of nitrogenous waste in the form of uric acid. |
| ii. | Excretion of ammonia requires plenty of water. | Excretion of uric acid requires negligible amount of water. |
| iii. | Removal of 1 gm of ammonia requires 300 – 500 ml of water. | Removal of 1 gm of uric acid requires 10ml of water. |
| iv. | Ammonia is very toxic. | Uric acid is less toxic. |
| e.g. | It is found in aquatic invertebrates, bony fishes and aquatic/ larval amphibians, etc. | It is seen in birds, some insects, many reptiles, land snails, etc. |
[Students can Refer these and make a chart on their own.]
Use your brain power. (Textbook Page No. 178)
Question 1.
Creatinine is considered as index of kidney function. Give reason.
Answer:
- Plasma creatinine is produced from catabolism of creatinine phosphate during skeletal muscle contraction.
- It provides a ready source of high energy phosphate.
- Normally blood creatinine levels remain steady because the rate of production matches its excretion in urine.
- Hence, plasma creatinine is used as an index of kidney function and its level above normal is an indication of poor renal function.
[Note: Plasma creatinine is a waste product produced by muscles from the breakdown of a compound called ‘creatine phosphate ’.]
Make a table. (Textbook Page No. 178)
Question 1.
The excretory organs found in various animal phyla.
Answer:
| Sr. No. | Animal Phyla | Excretory organs |
| i. | Porifera | Lack excretory organ instead rely on water transport system/ Canal system |
| ii. | Coelenterata | Lack specialised excretory organs. Excretion takes place through simple diffusion or through the mouth. |
| iii. | Ctenophora | Lack specialised excretory organs |
| iv. | Platyhelminthes | Protonephridia or Flame cells |
| v. | Aschelminthes | Excretory tube and pore |
| vi. | Annelida | Nephridia |
| vii. | Arthropoda | Malpighian tubules |
| viii. | Mollusca | Organ of Bojanus |
| ix. | Echinodermata | Lack specialized excretory organs, waste materials directly diffuse into water or are excreted through tube feet |
| x. | Hemichordata | Proboscis gland |
| xi. | Chordata | Kidney |
Observe and complete. (Textbook Page No. 178)
Question 1.
Label the diagram and complete following paragraphs.
i. Kidney: A pair of ____ shaped kidneys are present on either side of the ____ from 12th thoracic to 3rd lumbar vertebra. Kidneys are present behind ___. Hence are called retroperitoneal. Dimensions of
each kidney are 10 × ____ × ____ cms. Average weight is ___ g in males and 135 g in ____. Outer surface is ___ and inner is concave. Notch on the inner concave surface is called ___. Renal artery enters and renal vein as well as ureter leave the kidney through hilus. Each kidney has almost 1 million functional units called ___.
ii. Ureters: A pair of ureters arise from ___ of each kidney. Each ureter is a long muscular tube 25 – 30 cm in length. Ureters open into ___ by separate openings, which are not guarded by valves. They pass obliquely through the wall of urinary bladder. This helps in prevention of ___ of urine due to compression of ureters while bladder is filled.
iii. Urinary bladder: It is a median ___ sac. A hollow muscular organ, the bladder is situated in pelvic cavity posterior to pubic symphysis. At the base of the ___ there is a small inverted triangular area called trigone. At the apex of this triangle is opening of urethra. At the two points of the base of the triangle are openings of ureters. Urinary bladder is covered externally by peritoneum. Inner to peritoneum is muscular layer. It is formed by detrusor muscles which consist of three layers of smooth muscles. Longitudinal – circular – longitudinal respectively. Innermost layer is made up of transitional ___. It helps bladder to stretch.
iv. Urethra: It is a ___ structure arising from urinary bladder and opening to the exterior of the body.
There are ___ urethral sphincters between urinary bladder and urethra.
a. Internal sphincter: Made up of ___ muscles, involuntary in nature.
b. External sphincter: Made up of ___ muscles, voluntary in nature.
Answer: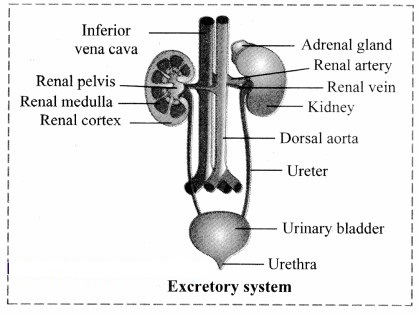
i. Kidney: A pair of bean shaped kidneys are present on either side of the backbone from 12th thoracic to 3rd lumbar vertebra. Kidneys are present behind peritoneum. Hence are called retroperitoneal. Dimensions of each kidney are 10 × 5 × 4 cms. Average weight is 150 g in males and 135 g in females. Outer surface is convex and inner is concave. Notch on the inner concave surface is called hilum. Renal artery enters and renal vein as well as ureter leave the kidney through hilus. Each kidney has almost 1 million functional units called nephron.
ii. Ureters: A pair of ureters arise from hilum of each kidney. Each ureter is a long muscular tube 25 – 30 cm in length. Ureters open into urinary bladder by separate openings, which are not guarded by valves. They pass obliquely through the wall of urinary bladder. This helps in prevention of backward flow of urine due to compression of ureters while bladder is filled.
iii. Urinary bladder: It is a median pear-shaped sac. A hollow muscular organ, the bladder is situated in pelvic cavity posterior to pubic symphysis. At the base of the urinary bladder there is a small inverted triangular area called trigone. At the apex of this triangle is opening of urethra. At the two points of the base of the triangle are openings of ureters. Urinary bladder is covered externally by peritoneum. Inner to peritoneum is muscular layer. It is formed by detrusor muscles which consist of three layers of smooth muscles. Longitudinal – circular – longitudinal respectively. Innermost layer is made up of transitional epithelial tissue. It helps bladder to stretch.
iv. Urethra: It is a fibromuscular tube-like structure arising from urinary bladder and opening to the exterior of the body. There are two urethral sphincters between urinary bladder and urethra.
a. Internal sphincter: Made up of detrusor muscles, involuntary in nature.
b. External sphincter: Made up of striated muscles, voluntary in nature.
If this valve is not functioning properly during inflammation of bladder, it can lead to kidney infection.
Internet is my friend. (Textbook Page No. 179)
Question 1.
Find out what is floating kidney.
Answer:
- Floating kidney or nephroptosis, is an inferior displacement or dropping of the kidney.
- This condition occurs when the kidney slips from its normal position because it is not held securely in place by the adjacent organs or its fat covering.
- It generally develops in extremely thin people whose adipose capsule or renal fascia is deficient.
- It may result in twisting of the ureter and cause blockage of urine flow. The resulting backup of urine would put pressure on the kidney and damage the tissues.
- Twisting of the ureter may also cause pain and discomfort.
- This condition is more common in females than males and happens commonly among one in four people.
- Weakening of the fibrous bands that hold the kidney in place can predispose to floating kidney.
Can you recall? (Textbook Page No. 179)
Question 1.
Observe the figure carefully and label various regions of L.S. of kidney.
Answer: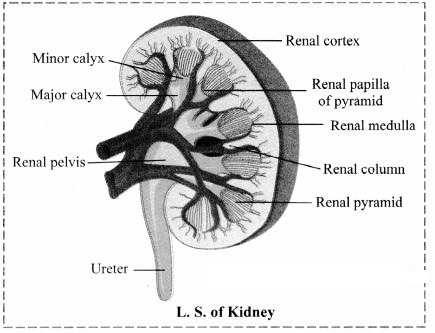
Can you tell? (Textbook Page No.182)
Question 1.
Why are kidneys called ‘retroperitoneal’?
Answer:
Kidneys are located in abdomen. Kidneys are not surrounded by peritoneum instead they are located posterior to it. Thus, kidneys are called retroperitoneal.
Question 2.
Why urinary tract infections are more common in females than males?
Answer:
- The urethra in women (4 cm) is much shorter than that of males (20 cm).
- This allows easy passage of bacteria into the urinary bladder.
Hence, urinary tract infections are more common in females than males.
Question 3.
What is nephron? Which are its main parts? Why are they important?
Answer:
Nephron is the structural and functional unit of kidney.
Structure of nephron:
A nephron (uriniferous tubule) is a thin walled, coiled duct, lined by a single layer of epithelial cells. Each nephron is divided into two main parts:
i. Malpighian body
ii. Renal tubule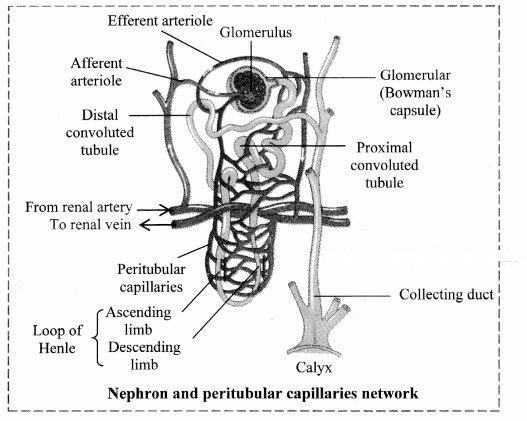
i. Malpighian body: Each Malpighian body is about 200pm in diameter and consists of a Bowman’s capsule and glomerulus.
a. Glomerulus:
Glomerulus is a bunch of fine blood capillaries located in the cavity of Bowman’s capsule.
A small terminal branch of the renal artery, called as afferent arteriole enters the cup cavity (Bowman capsule) and undergoes extensive fine branching to form network of several capillaries. This bunch is called as glomerulus.
The capillary wall is fenestrated (perforated).
All capillaries reunite and form an efferent arteriole that leaves the cup cavity.
The diameter of the afferent arteriole is greater than the efferent arteriole. This creates a high hydrostatic pressure essential for ultrafiltration, in the glomerulus.
b. Bowman’s capsule:
It is a cup-like structure having double walls composed of squamous epithelium.
The outer wall is called as parietal wall and the inner wall is called as visceral wall.
The parietal wall is thin consisting of simple squamous epithelium.
There is a space called as capsular space / urinary space in between two walls.
Visceral wall consists of special type of squamous cells called podocytes having a foot-like pedicel. These podocytes are in close contact with the walls of capillaries of glomerulus.
There are small slits called as filtration slits in between adjacent podocytes.
ii. Renal tubule:
a. Neck:
The Bowman’s capsule continues into the neck. The wall of neck is made up of ciliated epithelium. The lumen of the neck is called the urinary pole. The neck leads to proximal convoluted tubule.
b. Proximal Convoluted Tubule :
This is highly coiled part of nephron which is lined by cuboidal cells with brush border (microvilli) and surrounded by peritubular capillaries. Selective reabsorption occurs in PCT. Due to convolutions (coiling), filtrate flows slowly and remains in the PCT for longer duration, ensuring that maximum amount of useful molecules are reabsorbed.
c. Loop of Henle :
This is ‘U’ shaped tube consisting of descending and ascending limb.
The descending limb is thin walled and permeable to water and lined with simple squamous epithelium.
The ascending limb is thick walled and impermeable to water and is lined with simple cuboidal epithelium.
The LoH is surrounded by capillaries called vasa recta.
Its function is to operate counter current system – a mechanism for osmoregulation.
The ascending limb of Henle’s loop leads to DCT.
d. Distal convoluted tubule:
This is another coiled part of the nephron.
Its wall consists of simple cuboidal epithelium.
DCT performs tubular secretion / augmentation / active secretion in which, wastes are taken up from surrounding capillaries and secreted into passing urine.
DCT helps in water reabsorption and regulation of pH of body fluids.
e. Collecting tubule:
This is a short, straight part of the DCT which reabsorbs water and secretes protons.
The collecting tubule opens into the collecting duct.
Think about ¡t. (Textbook Page No. 182)
Question 1.
How much blood ¡s supplied to kidney?
Answer:
Around 600 ml of blood passes through each kidney per minute.
Do this. (Textbook Page No. 183)
Question 1.
Check blood reports of patients and comment about possibility of glucosuria.
Answer:
Glucosuria is the presence of glucose sugar in urine. High glucose in urine is usually indicative of diabetes mellitus.
| Condition | Glucose range in urine |
| Normal | 0 to 15 mg/dL (0 to 0.8 mmol/L) |
| Prediabetes | 100 to 125 mg/dL (5.6 to 6.9 mmol/L) |
| Diabetes | 126 mg/dL (7 mmol/L) |
[Students can get access to sample reports on the internet and refer the above table to comment on blood reports of patients on their own.]
Use your brain power. (Textbook Page No. 185)
Question 1.
In which regions of nephron the filtrate will he isotonic to blood?
Answer:
Filtrate leasing the proximal convoluted tubule (PCT) is isotonic to the blood plasma.
Can you tell? (Textbook Page No. 185)
Question 1.
Explain the process of urine formation in details.
Answer:
Process of urine formation is completed in three steps, namely;
i. Ultrafiltration/ Glomerular filtration,
ii. Selective reabsorption,
iii. Tubular secretion / Augmentation
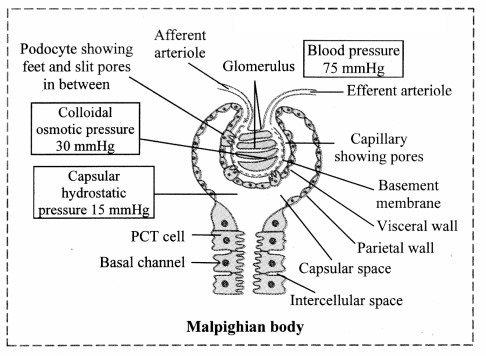
i. Ultrafiltration / Glomerular filtration :
Diameter of afferent arteriole is greater than the efferent arteriole. The diameter of capillaries is still smaller than both arterioles. Due to the difference in diameter, blood flows with greater pressure through the glomerulus. This is called as glomerular hydrostatic pressure (GHP) and normally, it is about 55 mmHg. GIIP is opposed by osmotic pressure of blood (normally, about 30 mm Hg) and capsular pressure (normally, about 15 mm Hg).
Hence net / effective filtration pressure (EFP) is 10 mm Hg.
EFP = Hydrostatic pressure in glomerulus – (Osmotic pressure of blood + Filtrate Hydrostatic pressure)
= 55 – (30 + 15)
= 10 mm Hg
Under the effect of high pressure, the thin walls of the capillary become permeable to major components of blood (except blood cells and macromolecules like protein).
Thus, plasma except proteins oozes out through wall of capillaries.
About 600 ml blood passes through each kidney per minute.
The blood (plasma) flowing through kidney (glomeruli) is filtered as glomerular filtrate, at a rate of 125 ml / min. (180 L/d).
Glomerular filtrate / deproteinized plasma / primary urine is alkaline, contains urea, amino acids, glucose, pigments, and inorganic ions.
Glomerular filtrate passes through filtration slits into capsular space and then reaches the proximal convoluted tubule.
ii. Selective reabsorption :
Selective reabsorption occurs in proximal convoluted tubule (PCT). It is highly coiled so that glomerular filtrate passes through it very slowly. Columnar cells of PCT are provided with microvilli due to which absorptive area increases enormously.
This makes the process of reabsorption very effective.
These cells perform active (ATP mediated) and passive (simple diffusion) reabsorption.
Substances with considerable importance (high threshold) like – glucose, amino acids, vitamin C, Ca++, K+, Na+, Cl– are absorbed actively, against the concentration gradient. Low threshold substances like water, sulphates, nitrates, etc., are absorbed passively.
In this way, about 99% of glomerular filtrate is reabsorbed in PCT and DCT.
iii. Tubular secretion / Augmentation :
Finally filtrate reaches the distal convoluted tubule via loop of Henle. Peritubular capillaries surround DCT. Cells of distal convoluted tubule and collecting tubule actively absorb the wastes like creatinine and ions like K+, H+ from peritubular capillaries and secrete them into the lumen of DCT and CT, thereby augmenting the concentration of urine and changing its pH from alkaline to acidic.
Secretion of H+ ions in DCT and CT is an important homeostatic mechanism for pH regulation of blood. Tubular secretion is the only process of excretion in marine bony fishes and desert amphibians.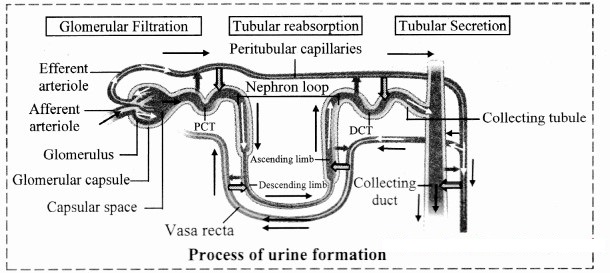
Question 2.
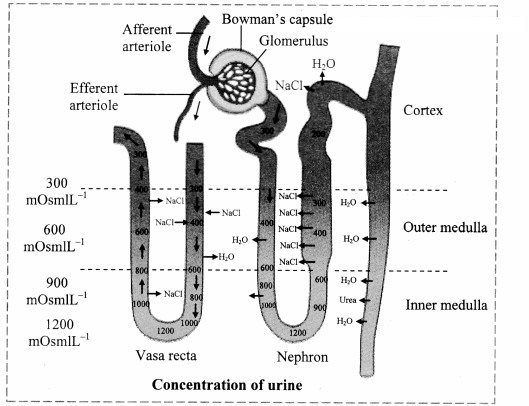
How does counter current mechanism help concentration of urine?
Answer:
Under the conditions like low water intake or high water loss due to sweating, humans can produce concentrated urine. This urine can be concentrated around four times i.e. 1200 mOsm/L than the blood (300 mOsm/L). Hence, a mechanism called countercurrent mechanism is operated in the human kidneys. The countercurrent mechanism operating in the Limbs of Henle’s loop of juxtamedullary nephrons and vasa recta is as follows:
- It involves the passage of fluid from descending to ascending limb of Henle’s loop.
- This mechanism is called countercurrent mechanism, since the flow of tubular fluid is in opposite direction through both limbs.
- In case of the vasa recta, blood flows from ascending to descending parts of itself.
- Wall of descending limb is thin and permeable to water, hence, water diffuses from tubular fluid into tissue fluid due to which, tubular fluid becomes concentrated.
- The ascending limb is thick and impermeable to water. Its cells can reabsorb Na+ and Cl– from tubular fluid and release into tissue fluid.
- Due to this, tissue fluid around descending limb becomes concentrated. This makes more water to move out from descending limb into tissue fluid by osmosis.
- Thus, as tubular fluid passes down through descending limb, its osmolarity (concentration) increases gradually due to water loss and on the other hand, progressively decreases due to Na+ and Cl– secretion as it flows up through ascending limb.
- Whenever retention of water is necessary, the pituitary secretes ADH. ADH makes the cells in the wall of collecting ducts permeable to water.
- Due to this, water moves from tubular fluid into tissue fluid, making the urine concentrated.
- Cells in the wall of deep medullar part of collecting ducts are permeable to urea. As concentrated urine flows through it, urea diffuses from urine into tissue fluid and from tissue fluid into the tubular fluid flowing through thin ascending limb of Henle’s loop.
- This urea cannot pass out from tubular fluid while flowing through thick segment of ascending limb, DCT and cortical portion of collecting duct due to impermeability for it in these regions.
- However, while flowing through collecting duct, water reabsorption is operated under the influence of ADII. Due to this, urea concentration increases in the tubular fluid and same urea again diffuses into tissue fluid in deep medullar region.
- Thus, same urea is transferred between segments of renal tubule and tissue fluid of inner medulla. This is called urea recycling; operated for more and more water reabsorption from tubular fluid and thereby excreting small volumes of concentrated urine.
- Osmotic gradient is essential in the renal medulla for water reabsorption by counter current multiplier system.
- This osmotic gradient is maintained by vasa recta by operating counter current exchange system.
- Vasa recta also have descending and ascending limbs. Blood that enters the descending limb of the vasa recta has normal osmolarity of about 300 mOsm/L.
- As it flows down in the region of renal medulla where tissue fluid becomes increasingly concentrated, Na+, Cl– and urea molecules diffuse from tissue fluid into blood and water diffuse from blood into tissue fluid.
- Due to this, blood becomes more concentrated which now flows through ascending part of vasa recta. This part runs through such region of medulla where tissue fluid is less concentrated.
- Due to this, Na+, Cl– and urea molecules diffuse from blood to tissue fluid and water from tissue fluid to blood. This mechanism helps to maintain the osmotic gradient.

Try this. (Textbook Page No. 185)
Question 1.
Read the given urine report and prepare a note on composition of normal urine.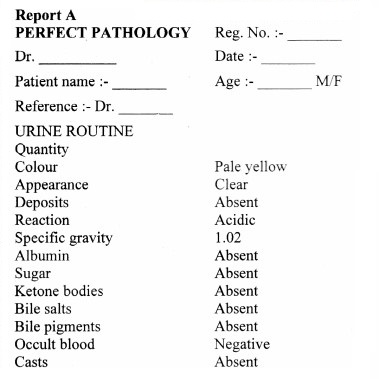
Answer:
The composition of normal urine is as follows:
- A volume of 1 – 2 litres of urine in 24 hours is normal. This volume can however vary considerably as it depends on fluid intake, physical activity, temperature, etc.
- The colour of normal urine is generally pale yellow due to urochrome (pigment produced by breakdown of bile). The colour of urine may vary slightly due to urochrome concentration and diet.
- The appearance of urine is generally clear and transparent.
- Any form of deposits (sediments/ crystals) is generally absent in normal urine.
- The pH of normal urine is acidic and is generally around 6.0 (Range: 4.6 to 8.0). The pH varies considerably with the diet of a person.
- The specific gravity of urine is an average of 1.02 ( Range : 1.001 to 1.035).
- Albumin, sugar, bile salts bile pigments, ketone bodies and casts are absent in normal urine.
- Occult blood is generally not seen in normal urine.
Think (Textbook Page No. 185)
Question 1.
What would happen if ADH secretion decreases due to any reason?
Answer:
In absence of ADH, diuresis (dilution of urine) takes place and person tends to excrete large amount of dilute urine. This condition called as diabetes insipidus. Frequent excretion of large amount of dilute urine may cause a person to feel thirsty.
Think and appreciate. (Textbook Page No. 185)
Question 1.
How do kidneys bring about homeostasis? Is there any role of neuro endocrine system in it?
Answer:
The composition of urine depends upon food and fluid consumed by an individual. There are two ways in which it the composition is regulated. They are as follows:
i. Regulating water reabsorption through ADH
ii. Electrolyte reabsorption though RAAS
iii. Atrial Natriuretic Peptide
i. Regulating water reabsorption through ADH:
Hypothalamus in the midbrain has special receptors called osmoreceptors which can detect change in osmolarity (measure of total number of dissolved particles per liter of solution) of blood.
If osmolarity of blood increases due to water loss from the body (after eating namkeen or due to sweating), osmoreceptors trigger release of Antidiuretic hormone (ADH) from neurohypophysis (posterior pituitary). ADH stimulates reabsorption of water from last part of DCT and entire collecting duct by increasing the permeability of cells.
This leads to reduction in urine volume and decrease in osmolarity of blood.
Once the osmolarity of blood comes to normal, activity of osmoreceptor cells decreases leading to decrease in ADH secretion. This is called negative feedback.
In case of hemorrhage or severe dehydration too, osmoreceptors stimulate ADH secretion. ADH is important in regulating water balance through kidneys.
In absence of ADH, diuresis (dilution of urine) takes place and person tends to excrete large amount of dilute urine. This condition called as diabetes insipidus.
[Note: Hypothalamus is a part of forebrain]
ii. Electrolyte reabsorption through RAAS:
Another regulatory mechanism is RAAS (Renin Angiotensin Aldosterone System) by Juxta Glomerular Apparatus (JGA).
Whenever blood supply (due to change in blood pressure or blood volume) to afferent arteriole decreases (e.g. low BP/dehydration), JGA cells release Renin. Renin converts angiotensinogen secreted by hepatocytes in liver to Angiotensin I. ‘Angiotensin converting enzyme’ further modifies Angiotensin I to Angiotensin II, the active form of hormone. It stimulates adrenal cortex to release another hormone called aldosterone that stimulates DCT and collecting ducts to reabsorb more Na and water, thereby increasing blood volume and pressure.
iii. Atrial natriuretic peptide (ANP): A large increase in blood volume and pressure stimulates atrial wall to produce atrial natriuretic peptide (ANP). ANP inhibits Na+ and Cl– reabsorption from collecting ducts inhibits release of renin, reduces aldosterone and ADH release too. This leads to a condition called Natriuresis (increased excretion of Na+ in urine) and diuresis.
No. Both ADH and RAAS are essential for homeostasis.
- Only ADH can lower blood Na+ concentration by way of water reabsorption in DCI and collecting duct. whereas RAAS stimulates Na+ reabsorption and maintains osmolarity of body fluid.
- Action of ADH and RAAS leads to increase in blood volume and osmolarity.
- For mechanism of Atrial natriuretic peptide:
Atrial natriuretic peptide (ANP): A large increase in blood volume and pressure stimulates atrial wall to produce atrial natriuretic peptide (ANP). ANP inhibits Na+ and Cl– reabsorption from collecting ducts inhibits release of renin, reduces aldosterone and ADH release too. This leads to a condition called Natriuresis (increased excretion of Na+ in urine) and diuresis.
ADH is produced by the hypothalamus and is stored and released by the posterior pituitary or the neurohypophysis in response to appropriate trigger. Hence, there is a role of the neuroendocrine system in homeostasis.
Use your brain power. (Textbook Page No. 186)
Question 1.
Can we use this knowledge in treatment of high blood pressure? Why high BP medicines are many a times diuretics?
Answer:
- Yes, the knowledge of homoeostasis is used in the treatment of high blood pressure.
- Some commonly used theories for treatment of high blood pressure are as follows:
- Angiotensin II receptor blockers (ARBs) are used as medications to treat high blood pressure. These medications block the action of angiotensin II by preventing angiotensin II from binding to angiotensin II receptors on the muscles surrounding blood vessels. As a result, blood vessels enlarge (dilate), and blood pressure is reduced.
- Another method is the use of ‘Angiotensin converting enzyme’ ACE blockers. These inhibitors inhibit activity of ACE and therefore decrease the production of angiotensin II. As a result, these medications cause the blood vessels to enlarge or dilate, and this reduces blood pressure.
- Vasodilation reduces arterial pressure. Reduced angiotensin II leads to natriuresis (increased excretion of Na+ in urine) and diuresis, thereby reducing blood pressure.
- Too much salt can cause extra fluid to build up in the blood vessels, raising blood pressure. Diuretics are substances that slow renal absorption of water and thereby cause diuresis (elevated urine flow rate) which in turn reduces blood volume and blood pressure by flushing out salt and extra fluid. Hence, high BP medicines are many a times diuretics.
Can you tell? (Textbook page no. 186)
How do skin and lungs help in excretion?
OR
Can you tell? (Textbook page no. 187)
Explain role of lungs and skin in excretion.
Answer:
Yes, various organs other than the kidney participate in excretion. They are as follows:
i. Skin:
Skin acts as an accessory excretory organ. The skin of many organisms is thin and permeable. It helps in diffusion of waste products like ammonia.
Human skin however is thick and impermeable. It shows presence of two types of glands namely, sweat glands and sebaceous glands.
- Sweat glands are distributed all over the skin. They are abundant in the palm and facial regions.
These simple, unbranched, coiled, tubular glands open on the surface of the skin through an opening called sweat pore. Sweat is primarily produced for thermoregulation but it also excretes substances like water, NaCl, lactic acid and urea. - Sebaceous glands are present at the neck of hair follicles. They secrete oily substance called sebum.
It forms a lubricating layer on skin making it softer. It protects skin from infection and injury.
ii. Lungs:
Lungs are the accessory excretory organs. They help in excretion of volatile substances like CO2 and water vapour produced during cellular respiration. Along with CO2, lungs also remove excess of H2O in the form of vapours during expiration. They also excrete volatile substances present in spices and other food stuff.
Can you tell? (Textbook Page No. 187)
Question 1.
When does kidney produce renin? Where is it produced in kidney?
Answer:
Kidney produces renin whenever blood supply (due to change in blood pressure or blood volume) to afferent arteriole decreases (e.g. low BP/dehydration).
The juxtaglomerular Apparatus (JGA) cells secrete renin.
Question 2.
Explain how electrolyte balance of blood plasma maintained.
Answer:
The composition of urine depends upon food and fluid consumed by an individual. There are two ways in which it the composition is regulated. They are as follows:
i. Regulating water reabsorption through ADH
ii. Electrolyte reabsorption though RAAS
iii. Atrial Natriuretic Peptide
i. Regulating water reabsorption through ADH:
Hypothalamus in the midbrain has special receptors called osmoreceptors which can detect change in osmolarity (measure of total number of dissolved particles per liter of solution) of blood.
If osmolarity of blood increases due to water loss from the body (after eating namkeen or due to sweating), osmoreceptors trigger release of Antidiuretic hormone (ADH) from neurohypophysis (posterior pituitary). ADH stimulates reabsorption of water from last part of DCT and entire collecting duct by increasing the permeability of cells.
This leads to reduction in urine volume and decrease in osmolarity of blood.
Once the osmolarity of blood comes to normal, activity of osmoreceptor cells decreases leading to decrease in ADH secretion. This is called negative feedback.
In case of hemorrhage or severe dehydration too, osmoreceptors stimulate ADH secretion. ADH is important in regulating water balance through kidneys.
In absence of ADH, diuresis (dilution of urine) takes place and person tends to excrete large amount of dilute urine. This condition called as diabetes insipidus.
[Note: Hypothalamus is a part of forebrain]
ii. Electrolyte reabsorption through RAAS:
Another regulatory mechanism is RAAS (Renin Angiotensin Aldosterone System) by Juxta Glomerular Apparatus (JGA).
Whenever blood supply (due to change in blood pressure or blood volume) to afferent arteriole decreases (e.g. low BP/dehydration), JGA cells release Renin. Renin converts angiotensinogen secreted by hepatocytes in liver to Angiotensin I. ‘Angiotensin converting enzyme’ further modifies Angiotensin I to Angiotensin II, the active form of hormone. It stimulates adrenal cortex to release another hormone called aldosterone that stimulates DCT and collecting ducts to reabsorb more Na and water, thereby increasing blood volume and pressure.
iii. Atrial natriuretic peptide (ANP): A large increase in blood volume and pressure stimulates atrial wall to produce atrial natriuretic peptide (ANP). ANP inhibits Na+ and Cl– reabsorption from collecting ducts inhibits release of renin, reduces aldosterone and ADH release too. This leads to a condition called Natriuresis (increased excretion of Na+ in urine) and diuresis.
No. Both ADH and RAAS are essential for homeostasis.
- Only ADH can lower blood Na+ concentration by way of water reabsorption in DCI and collecting duct. whereas RAAS stimulates Na+ reabsorption and maintains osmolarity of body fluid.
- Action of ADH and RAAS leads to increase in blood volume and osmolarity.
- For mechanism of Atrial natriuretic peptide:
Atrial natriuretic peptide (ANP): A large increase in blood volume and pressure stimulates atrial wall to produce atrial natriuretic peptide (ANP). ANP inhibits Na+ and Cl– reabsorption from collecting ducts inhibits release of renin, reduces aldosterone and ADH release too. This leads to a condition called Natriuresis (increased excretion of Na+ in urine) and diuresis.
Can you tell? (Textbook Page No. 187)
Question 1.
What is the composition of sweat?
Answer:
Sweat is composed of water, NaCl, lactic acid and urea.
Internet my friend. (Textbook Page No. 189)
Question 1.
Treatments other than surgical removal of kidney stone like Lithotripsy. (Breaking down of kidney stones using shock waves).
Answer:
a. Cystoscopy and ureteroscopy:
During cystoscopy, the doctor uses a cystoscope to look inside the urethra and bladder to find a stone in the urethra or bladder.
During ureteroscopy, the doctor uses a ureteroscope, which is longer and thinner than a cystoscope, to see detailed images of the lining of the ureters and kidneys.
The doctor inserts the cystoscope or ureteroscope through the urethra to see the rest of the urinary tract. Once the stone is found, the doctor can remove it or break it into smaller pieces.
The doctor performs these procedures in the hospital with anesthesia.
b. Percutaneous nephrolithotomy:
The doctor uses a thin viewing tool, called a nephroscope, to locate and remove the kidney stone.
The doctor inserts the tool directly into your kidney through a small cut made in your back.
For larger kidney stones, the doctor also may use a laser to break the kidney stones into small pieces. The doctor performs percutaneous nephrolithotomy in a hospital with anesthesia.
c. Generally for smaller stones doctors recommend drinking lots of water, consuming pain relievers and consuming medicines like alpha blocker to relax the ureter muscles, and help pass the kidney stones more quickly and with less pain
[Students are expected to find more information using the internet.]
Question 2.
Dietary restrictions suggested for kidney patients.
Dietary restrictions for kidney patients include the following:
- Drinking large amounts of water.
- Reduce consumption of oxalate rich food like rhubarb, beets, okra, spinach, Swiss chard, sweet potatoes, nuts, tea, chocolate and soy products.
- Follow a diet low in salt and animal protein.
- Reduce consumption of calcium supplements (if any) but consume appropriate amount of calcium in food.
[Students are expected to find more information using the internet.]